Continuing Education
Join the RESPTREC® family for lifelong learning opportunities and mentorship.
Professional Education Portal
Lung Sask in collaboration with RESPTREC® offers the Professional Education Portal as a method for respiratory educators and health care providers to enhance their professional learning with continuing education opportunities.
Read articles and watch video presentations on the most recent research, position papers and guidelines. Track your CE hours with the provided logbook.
RESPTREC® resources
Download or order branded resources for your workplace:
- Asthma Medications Brochure
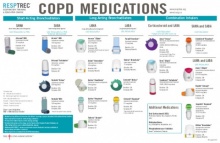
- COPD Medications Brochure
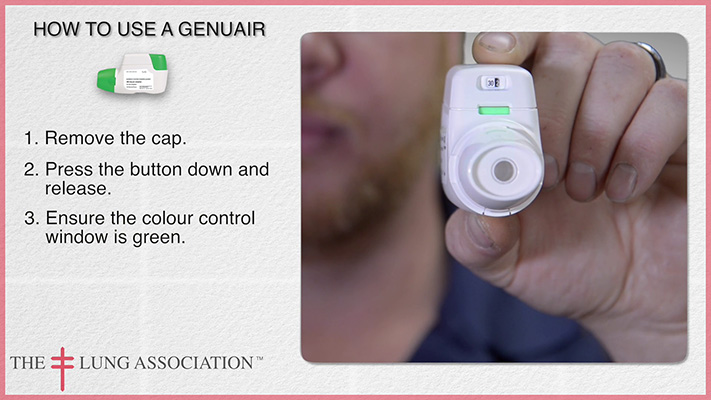
- Delivery Device Instructions
- Delivery Device Mastery Sheets
- Inhaler Device Demonstration Videos
Recent News & Articles
For your convenience the Professional Education Portal & RESPTREC® provide links to research articles, announcements, studies and other news updates which are posted daily onto the website.
Reading these articles can be used towards recertification and continuing education.
Advancing assessment of asthma control with a composite tool
Apr 22, 2024
Relative to other control tools and expert opinion informed by GINA 4-question symptom control tool and risk factors for poor asthma outcomes, the composite Asthma Impairment and Risk Questionnaire performs better in assessing both domains of current control and predicting exacerbation risk.
Antibiotics Not Associated with Shorter Duration or Reduced Severity of Acute Lower Respiratory Tract Infection
Apr 16, 2024
In this large prospective study in the US primary and urgent care setting, antibiotics had no measurable impact on the severity or duration of cough due to acute LRTI. Patients had unrealistic expectations regarding the duration of LRTI and the effect of antibiotics which should be the target of antibiotic…
Temporal Risk of Nonfatal Cardiovascular Events After COPD Exacerbation
Apr 15, 2024
Cardiovascular events after moderate COPD exacerbations occur slightly later than after severe exacerbations; heightened relative rates remain beyond one year irrespective of severity. The period immediately after an exacerbation presents a critical opportunity for clinical intervention and treatment optimization to prevent future cardiovascular events.
Over 5000+ more articles available in the Professional Education Portal. Track your CE time with the provided logbook.